Table of Contents
Heart disease is often dubbed a “man’s disease,” but since it is the leading cause of death for women in the world, the perception couldn’t be further from the truth. Heart attack symptoms in women over 50 are often subtle and misunderstood, making early detection challenging. Presented as one of the most serious consequences of the disease, heart attacks typically strike all those women beyond 50 in somewhat singular and sadly oft-misunderstood ways. Identification of those unique symptoms in older women is critical since, in every case, an early intervention can be a lifesaver.
In this article, we take a deep dive into the causes, risk factors, heart attack symptoms, and preventive measures of heart attacks in women over 50. We will also debunk some common myths, informing our readers of how female biology and age each contribute to differing presentations of heart attacks.
What Is a Heart Attack?
A heart attack develops in one patch of the heart muscle when the flow of blood has been obstructed. Such blockages most frequently arise as a result of plaque formation inside the coronary arteries-a process known as atherosclerosis. Once deprived of oxygen, the heart muscle starts dying.
The mechanism remains the same for men or women, but the symptoms and risk profiles could differ quite substantially, especially if the woman is a little over fifty.
Why Focus on Women Over 50?
The risk of heart disease jumps up very sharply in a woman after she crosses 50-the normal time of menopause. As quoted by the CDC:
- One in five female deaths is caused by heart disease.
- Cholesterol and blood pressure increase much more at postmenopausal level and thereby raise the risk of heart disease.
- Women have more chances of dying once they have suffered a heart attack.
At this age group, symptoms tend to be atypical; are not the normal textbook chest pain in general; hence they are difficult to comfort and diagnose in an early stage.
Unique Symptoms of Heart Attack in Women Over 50
Women over 50 often experience “atypical” or subtle symptoms, which can be confused with less serious conditions.
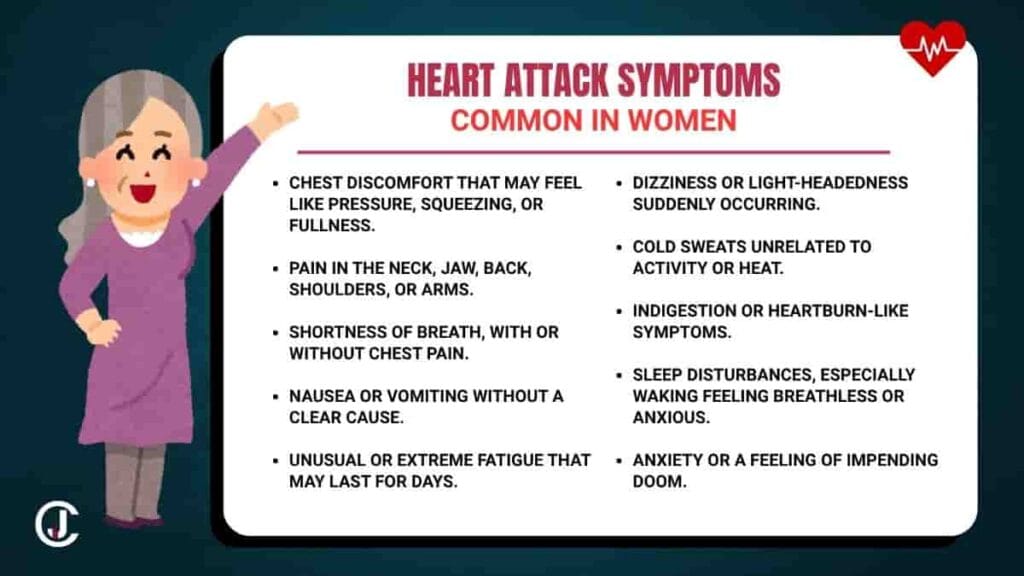
Common Symptoms in Women:
| Symptom | Description |
| Unusual fatigue | Sudden, unexplained exhaustion lasting days. |
| Shortness of breath | Difficulty breathing, even without exertion. |
| Chest discomfort | Tightness, pressure, or squeezing—not necessarily pain. |
| Nausea and vomiting | Often mistaken for indigestion or a stomach bug. |
| Back, neck, jaw, or shoulder pain | Pain radiating without any physical strain. |
| Dizziness or light-headedness | May be accompanied by anxiety or cold sweats. |
| Sleep disturbances | Unusual difficulty falling or staying asleep. |
These symptoms may occur gradually or suddenly and are often mistaken for anxiety, flu, or menopause.
Commonly Misinterpreted Signs
Because symptoms like fatigue or indigestion are nonspecific, women frequently:
- To seek help on the assumption that it is not serious.
- To make a wrong self-diagnosis, especially in the absence of chest pain.
- To be incorrectly diagnosed by health professionals, especially at emergency settings.
This delay in treatment leads to a high probability for death and complication.
Biological and Hormonal Differences
Female hormones play a key role in how heart attacks present.
Estrogen’s Protective Role
From birth till menopause, estrogen serves to keep arteries flexible and cholesterol levels in check. Postmenopause:
- Estrogen decreases, and this gives rise to an accumulation of plaques.
- Blood vessels lose their elasticity, thus having an effect on blood pressure.
- Increase in inflammatory markers that predispose to heart disease.
Smaller Coronary Arteries
Women have narrower vessels which can be obstructed more easily and do not show up well on the standard diagnostic tests.
Risk Factors for Heart Attack in Older Women
Traditional Risk Factors
- High blood pressure
- High LDL (“bad”) cholesterol
- Diabetes
- Smoking
- Obesity
- Family history of heart disease
- Physical inactivity
Female-Specific Risk Factors
- Early menopause
- Polycystic ovary syndrome (PCOS)
- Pregnancy-related conditions (e.g., preeclampsia, gestational diabetes)
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis)
Psychosocial Factors
- Chronic stress
- Depression
- Social isolation
Women are twice as likely as men to experience depression, which has a direct impact on heart health.
Diagnostic Challenges in Women
Atypical Symptoms = Delayed Diagnosis
Doctors are trained to look for classic chest pain as the hallmark of a heart attack. When a woman presents with back pain, fatigue, or nausea, the connection is often missed.
Gender Bias in Medicine
Studies show that women are:
- Less likely to receive prompt ECGs or troponin tests.
- Less likely to be referred for angiography or cardiac catheterization.
- More likely to be sent home from the ER without treatment.
False Negatives in Testing
Due to smaller arteries and microvascular disease, angiograms may look “normal” in women even when blood flow is impaired.
The Role of Menopause
Menopausal transition very much influences the cardiovascular system.
Major Changes:
- Increase in LDL cholesterols and triglycerides
- Decrease in HDL cholesterol (good cholesterol)
- Increase in abdominal fats and insulin resistance
- Vascular stiffness and rising blood pressure
Use of Hormones Replacement Therapy (HRT)
This type of treatment was once considered protective of the heart, but the new studies come up with varied findings. The American Heart Association discourages the use of HRT for the prevention of heart diseases but considers it in selected cases of menopausal symptom relief.
Silent Heart Attacks: The Hidden Threat
A silent heart attack, by definition, is an attack that is usually not recognized, undiagnosed or untreated due to lack of any overt or evident clinical symptoms. It occurs once every fifth occurrence of a heart attack, and according to statistics, women are more prone to experiencing it, especially past 50.
How to Identify a Silent Heart Attack:
- Atypical tiredness
- Mild indigestion or heartburn
- Back or jaw discomfort
- Sweating with no exertion, cold sweats
- Mild bouts of breathlessness or fainting spells
Many would remain unaware that these signals could be warnings of a silent heart attack and would more likely dismiss them as symptoms of tiredness or stress.
When to Seek Emergency Help
Act FAST if you notice:
- Sudden or persistent chest discomfort
- Pain in arms, back, neck, or jaw
- Shortness of breath
- Light-headedness or cold sweat
- Nausea or vomiting
- A sense of doom or anxiety that is out of proportion
Call Emergency Services Immediately.
Do not drive yourself to the hospital. Take aspirin if advised, and wait for paramedics to assist.
Preventing Heart Attacks: Lifestyle and Medical Tips
Lifestyle Strategies
| Strategy | Benefit |
| Exercise (30 min/day) | Lowers blood pressure and cholesterol |
| Heart-healthy diet (DASH or Mediterranean) | Reduces inflammation and plaque buildup |
| Quit smoking | Cuts heart disease risk by 50% in one year |
| Stress reduction (yoga, meditation) | Lowers cortisol, improves sleep |
| Limit alcohol | Excess drinking can raise BP and cause arrhythmias |
| Weight management | Reduces strain on the heart |
Medical Interventions
- Routine health screenings (cholesterol, blood pressure, glucose)
- Medications as prescribed: statins, beta-blockers, ACE inhibitors
- Regular cardiac check-ups if you have a family history
- Control of co-existing conditions like diabetes or arthritis
FAQs: Women’s Heart Health
Q1: Are heart attack symptoms in women always different?
Not always, but they are more likely to present atypically—especially in older women.
Q2: Can menopause cause heart attacks?
Menopause, per se, does not cause heart attacks but brings in an increased cardiovascular risk due to hormonal imbalance.
Q3: How can I tell if it’s anxiety or a heart issue?
If you experience unusual fatigue, pressure in the chest, or breathlessness, always err on the side of caution and get evaluated.
Q4: Are women more likely to die from a heart attack?
Largely, Yes. Women above fifty years of age do not recognize early symptoms even more, so that delayed treatment increases the mortality level.
Final Thoughts
Heart attacks in women over 50 are under-recognized, under-diagnosed, and under-treated. Just a little awareness about atypical symptoms like exhaustion, back pain, and nausea can actually save lives. Women should really embrace being proactive about heart health, especially before, during, and after menopause, because risk factors really pile up.
Stay in the loop, assert your needs, and don’t ever hesitate to rush yourself to the ER if something doesn’t feel right for your heart. Your heart matters, at any age.


2 thoughts on “Heart Attack Symptoms in Women Over 50: What Every Woman Should Know”